The Truth About Hormone Replacement Therapy Pellets
Hormone pellets have become a popular treatment marketed as a convenient, long-lasting way to optimize hormones and address hormonal imbalances. The idea sounds appealing: a quick procedure every few months, no daily medication to remember, and promises of “steady levels.” But while pellet therapy has grown in popularity, the research behind it has not kept pace. Many patients are never fully informed about how pellets work, the risks involved, or why this therapy can lead to unpredictable and sometimes problematic results. This guide breaks down what hormone replacement therapy pellets are, why they seem so attractive, and the concerns patients often are not told about. The goal is simple: to give you the information you deserve so you can make the safest, most informed decision for your health.
Understanding Hormone Pellets
Hormone pellets are small, compressed cylinders containing hormones, often testosterone alone or a blended formulation, that are surgically inserted under the skin in the upper buttock or hip area. They are marketed to dissolve over 3 to 6 months, releasing hormones into the bloodstream as the pellet breaks down. Although pellets are widely used, high-quality research specifically on compounded pellets is limited, and major medical societies such as the Endocrine Society, AACE, and NAMS do not recommend pellet therapy as a first-line approach. These organizations instead favor titratable and reversible forms of hormone replacement therapy because of their proven safety profile and adjustability.
Understanding the Appeal of Pellets
Pellets are often presented as the “easy” option. The perceived benefits make sense:
A few procedures per year
No daily pills, patches, or injections
Promises of “steady,” “natural,” or “bioidentical” hormones
For individuals struggling with fatigue, low libido, weight changes, mood symptoms, menopause, or low testosterone, this can look like a simple solution. But what many patients do not realize is that pellets are not the only low-maintenance option, and they are not the most predictable or safest choice based on available data.
Pellet Pharmacology: How They Work
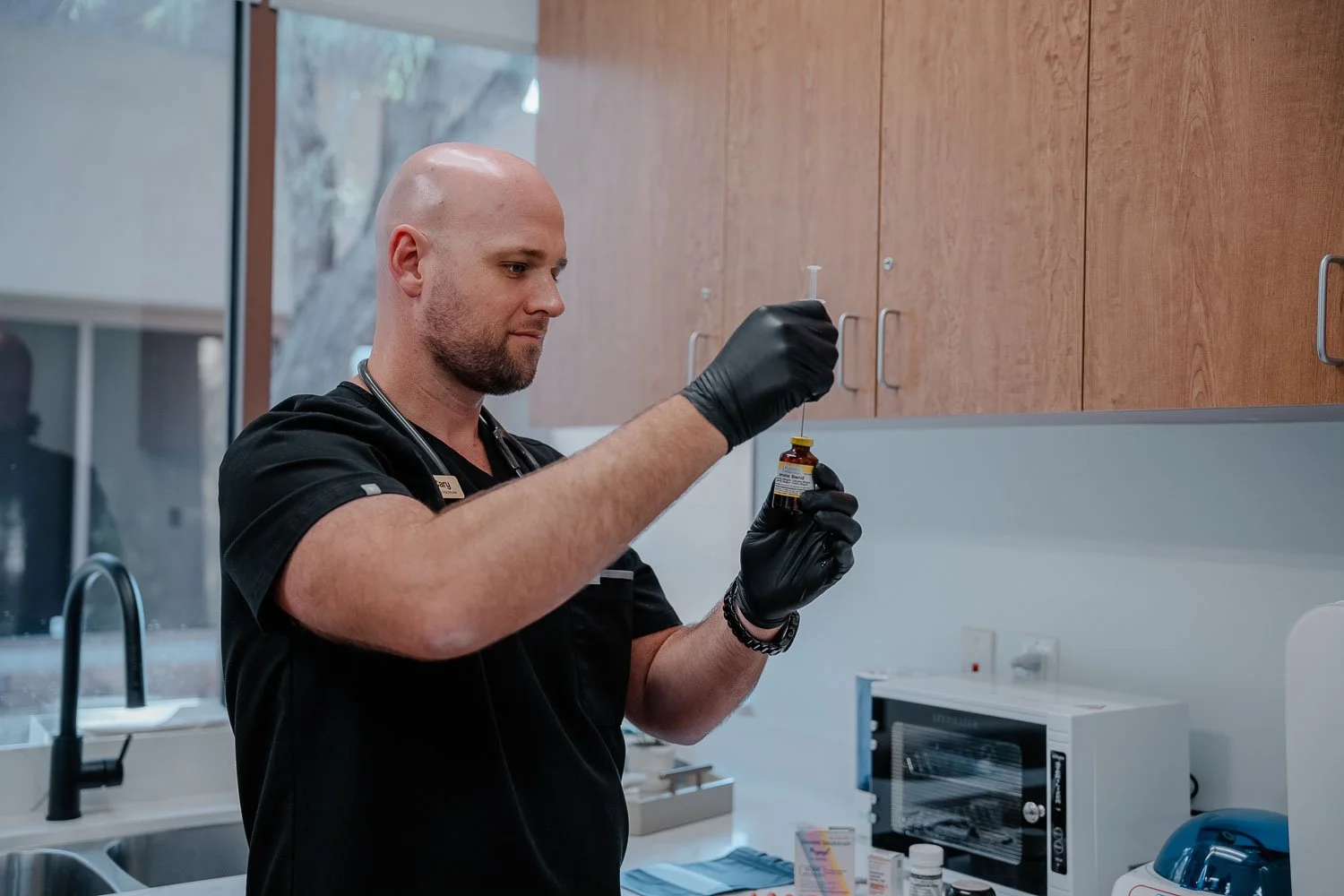
Procedure Overview
Pellet therapy involves making an incision, placing the pellets into subcutaneous fat, and closing or bandaging the site. Like any implantable procedure, it carries risks such as infection, extrusion, and scarring.
Mechanism of Action
After insertion, pellets are intended to dissolve gradually over 3 to 6 months, releasing hormones continuously into the bloodstream.
Typical Hormone Pattern (rarely discussed upfront)
Pellets do not produce a flat, steady hormone release. Instead:
Levels rise rapidly after insertion
Levels decline gradually over months
This pattern can lead to:
Early peaks that cause symptoms of excess
Late troughs where symptoms return
Prolonged supraphysiologic levels, especially in lean individuals
This pattern is supported by the foundational PK study on testosterone pellets, showing rapid early peaks and a declining curve. Not every patient experiences the same pattern, but the variability makes timing labs and dosing difficult. Without proper testing before reinsertion, patients may unknowingly stay in unsafe ranges for extended periods.
Unpredictable Absorption
Pellet absorption depends heavily on:
Body fat
Physical activity
Blood flow
Depth and technique of insertion
Individual metabolism
The Concerns Patients Often Aren't Told About
The Dose Cannot Be Adjusted:
Once pellets are placed, the dose cannot be reduced or reversed. Although surgical removal is technically possible, it is rarely practical and often not recommended.
If hormone levels are too high or side effects develop, patients must wait for levels to decline naturally over months. The lack of controlled titration goes directly against guideline recommendations that hormone therapy be adjustable and maintain physiologic levels.
2. Peaks, Troughs & Rollercoaster Levels:
Early peaks can lead to:
Irritability
Acne
Mood swings
Breast tenderness
Fluid retention
Androgenic effects in women
Hair loss
Late troughs often bring back menopausal or low testosterone symptoms. The adverse effects listed above are well-documented in clinical literature.
3. Risks of Sustained Supraphysiologic Hormone Levels
For Women
Excess testosterone may cause:
Acne or oily skin
Chin hair growth
Scalp hair thinning
Mood swings or irritability
Voice deepening
Clitoral enlargement
Negative effects on cholesterol
Excess estrogen, often from aromatization of high testosterone, may cause:
Breast tenderness
Bloating
Headaches
Heavy or irregular bleeding
Worsening migraines
For Men
High testosterone may cause:
Worsening sleep apnea
Acne
Irritability or aggression
Hair loss
Weight gain
Testicular atrophy
Elevated estradiol may cause:
Breast tenderness
Gynecomastia
Emotional swings
Fluid retention
4. Procedure Related Risks
Pellet extrusion
Infection or abscess
Bruising, hematoma, or bleeding
Persistent scar tissue
Pain or discomfort at the insertion site
The Real Price of Pellet Therapy
Although pellets appear convenient, the drawbacks often outweigh the benefits. When considering hormone replacement therapy cost, it's important to understand the full value of evidence-based alternatives.
Advantages of Evidence-Based Alternatives
Other therapies offer:
Predictable absorption
Ability to adjust dose quickly based on symptoms and lab values in real time
Strong clinical safety data
Lower risk of peaks and troughs
Lower overall cost
The Endocrine Society explicitly prefers therapies with predictable pharmacokinetics and reversible dosing. Comparative safety analyses confirm this.
Standard Hormone Therapy Options
Injectable testosterone
Oral micronized progesterone
Transdermal estrogen therapies
Troches and sublingual formulations
Compared to these options, pellets:
Cost more
Offer less dose flexibility
Are less consistent, making individualized dosing difficult
Are less individualized
Lack strong outcome data
Preferred Methods for Hormone Optimization
Understanding how to fix a hormonal imbalance effectively starts with choosing the right delivery method.
For Women
Troche formulations
SQ or IM injections, 2 to 3 times weekly
Oral micronized progesterone
Transdermal estradiol
Low dose testosterone, topical or injectable
For Men
Testosterone injections, typically 2 or 3 times weekly for level stability
Transdermal testosterone when appropriate
These methods allow precise titration, close monitoring, and safer long-term outcomes.
Transition Off Pellet Therapy: A Patient Guide
If you are on pellets now, there is no need to panic. Transitioning off pellets is very manageable with the right plan.
Typical Transition Steps
Allow pellets to wear off naturally
Check labs at the correct intervals
Track symptoms as levels change
Avoid additional pellet insertions
Begin short-acting, adjustable therapies once levels fall
Re-establish balance with physiologic, titratable dosing
Injx Bar’s Approach
At Injx Bar, hormone therapy is grounded in evidence-based practices and personalized dosing. We emphasize:
Scientifically supported delivery methods
Lab-guided decision-making
Safe, reversible therapies
Consistent monitoring
Treatment tailored to your physiology, not guesswork
Our approach aligns with the leading professional society guidelines. Our goal is to help patients feel and function their best with precision, predictability, and a fully individualized plan. And if you’re ready to feel more energized, more balanced, and more like yourself again, reach out today to schedule a consultation. Let’s create a plan that helps your hormonal imbalances finally feel manageable in a way that fits your life.